Airway obstruction
| Airway obstruction | |
|---|---|
| Specialty | Pulmonology |
Airway obstruction is a blockage of respiration in the airway that hinders the free flow of air. Airway obstructions can occur either in the upper airway (UPA) or lower airway (LOA). The upper airway consists of the nose, throat, and larynx. The lower airway comprises the trachea, bronchi, and bronchioles. [1]

Airway obstruction is a life-threatening condition and requires urgent attention, and assistance when it is needed.[2]
Upper airway obstruction
[edit]Causes
[edit]The causes of upper airway obstructions can be acute or chronic. More acute causes of upper airway obstruction include foreign body aspiration, blunt trauma to the neck, infections, and swelling due to allergies or other inflammatory conditions.[3] In children, viral infections such as croup or epiglottitis are frequent causes.[4] Adults are more likely to experience obstruction from enlargement of the tonsils or vocal cord paralysis. [3] Obstructive sleep apnea is the most common chronic cause of upper airway obstruction.[2]
Symptoms
[edit]It is possible to determine where the obstruction is based on the patient's symptoms. Stridor is a high-pitched sound which occurs during breathing and is associated with obstruction at the level of the larynx. Difficulty swallowing and changes in voice are also common symptoms.[3] If there is total obstruction, severe respiratory distress or cyanosis due to hypoxia (lack of oxygen in the blood) can occur.[2]
Diagnosis
[edit]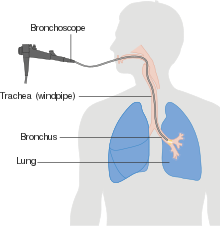
It is crucial to determine if a patient has an acute upper airway obstruction. Respiratory distress can rapidly lead to respiratory failure without appropriate management.[2] Thus, the first step is to conduct an urgent and comprehensive assessment of ABCs (airway, breathing, and circulation).[1]
Imaging studies can also help with diagnosis. First-line imaging studies include x-rays and CT scans. They can quickly assess the obstruction's extent.[2] For children, ultrasound or MRI are preferred as they do not involve radiation.[5] Flexible laryngoscopy or bronchoscopy can directly visualize the airway.[2]
Management
[edit]Treatment depends on how severe the patient's condition is and the cause of the obstruction.

If the patient is choking on a foreign body, the Heimlich maneuver should be initiated. More invasive methods, such as intubation, may be necessary to secure the airway. In severe cases, intubation may be difficult. Thus, a cricothyrotomy or tracheostomy may be necessary.[2][6]
Infections typically cause obstruction by swelling. So, they are usually treated with antibiotics or corticosteroids to reduce inflammation.[1] For causes like tumors or abscesses, surgical intervention may be required for removal. [2]
Prognosis and Outcomes
[edit]The prognosis depends on the cause and rapidity of intervention. With prompt treatment, outcomes are usually favorable. This is especially true for reversible conditions, like foreign body aspiration.[2] Chronic conditions, like vocal cord paralysis and sleep apnea,[7] may need ongoing care. If managed well, they usually have good outcomes.
Complications
[edit]Untreated or prolonged upper airway obstruction can cause severe, life-threatening complications.
- Hypoxia: Low blood oxygen can cause confusion and unconsciousness. It can also lead to cardiac arrest if not fixed quickly.[1]
- Aspiration Pneumonia: If particles enter the lungs, it can cause lung infections. This can happen from aspirating a foreign body.[8]
- Structural Changes: Repeating obstruction or trauma may scar or narrow the upper airway. This is called subglottic or tracheal stenosis.[9]
- Voice Changes: Chronic damage to the vocal cords may cause permanent voice changes or loss.[1]
- Cardiac Arrest: Severe obstruction can cause asphyxiation, leading to heart failure if untreated.[8]
Lower airway obstruction
[edit]Causes
[edit]
Lower airway obstruction is mainly caused by increased resistance in the bronchioles. This is usually due to a decreased radius of the bronchioles. This typically occurs due to constriction and inflammation of the bronchioles. It reduces the air inhaled in each breath. This restriction is worsened by mucus production and airway remodeling in chronic conditions.[1] Diseases that cause lower airway obstruction are called obstructive lung diseases.[10] Examples include chronic obstructive pulmonary disease (COPD), asthma, and bronchitis.[11]
Symptoms
[edit]Patients often experience wheezing, shortness of breath, and a chronic cough. A wheeze is a coarse, whistling sound in the airways during breathing. Patients can have worsening of their symptoms called exacerbations. Exacerbations may include increased mucus production and reduced exercise tolerance.[11]
Diagnosis
[edit]
Spirometry is the gold standard for diagnosing lower airway obstruction. It measures the FEV1/FVC ratio. A decreased ratio indicates obstruction. [12]
Imaging can also help with the diagnosis. Chest X-rays can help exclude alternative diagnoses or include other comorbidities. CT images can also provide more insight into any possible structural abnormalities.[11]
Management
[edit]
Treatment of lower airway obstruction includes the following methods:
- Bronchodilators help relax and widen the airways, which improve the airflow.
- Inhaled corticosteroids help decrease airway inflammation.[11]
- Long-term oxygen therapy is usually reserved for more severe chronic cases.[9]
Severe cases may need hospitalization and mechanical ventilation. The ventilation helps support breathing by keeping the airways open.[9]
Prognosis and Outcomes
[edit]Prognosis depends on the severity and cause of the obstruction. With early diagnosis and treatment, conditions like asthma often have a good outcome. But, chronic diseases like COPD are progressive, requiring ongoing management.[11]
Complications
[edit]Lower airway obstruction, often from chronic diseases, has various complications:
- Chronic Hypoxia: Prolonged obstruction reduces oxygen supply. This leads to fatigue, confusion, and eventual organ damage. [1](Harrison's Principles of Internal Medicine, 20th Edition).
- Cor Pulmonale: Persistent low oxygen levels can strain the right side of the heart. This can lead to right-sided heart failure.[9] (Goldman-Cecil Medicine, 26th Edition).
- Frequent Infections: There is an increase risk of bacterial infections like pneumonia. (Harrison's Principles of Internal Medicine, 20th Edition).[1]
- Disease Progression: Chronic conditions, like asthma and COPD, can worsen over time. Poorly managed obstruction can cause severe disability and is associated with lung cancer.[1]
See also
[edit]References
[edit]- ^ a b c d e f g h i Loscalzo, Joseph; Fauci, Anthony; Kasper, Dennis; Hauser, Stephen; Longo, Dan; Jameson, Larry (2022). Harrison's Principles of Internal Medicine (21 ed.). McGraw Hill Education.
- ^ a b c d e f g h i Aboussouan, L.S.; Stoller, J.K (15 March 1994). "Diagnosis and management of upper airway obstruction". Clinics in Chest Medicine. 15 (1): 35–53. doi:10.1016/S0272-5231(21)01054-6. PMID 8200192. Archived from the original on 25 June 2021. Retrieved 25 June 2021.
- ^ a b c O Cathain, Eadaoin; Gaffey, Megan M. (2024), "Upper Airway Obstruction", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 33232069, retrieved 2024-10-31
- ^ Johnson, David Wyatt (2014-09-29). "Croup". BMJ Clinical Evidence. 2014: 0321. ISSN 1752-8526. PMC 4178284. PMID 25263284.
- ^ Ohana, Orly; Soffer, Shelly; Zimlichman, Eyal; Klang, Eyal (2018-05-01). "Overuse of CT and MRI in paediatric emergency departments". The British Journal of Radiology. 91 (1085). doi:10.1259/bjr.20170434. ISSN 0007-1285. PMC 6190788. PMID 29271231.
- ^ Apfelbaum, Jeffrey L.; Hagberg, Carin A.; Connis, Richard T.; Abdelmalak, Basem B.; Agarkar, Madhulika; Dutton, Richard P.; Fiadjoe, John E.; Greif, Robert; Klock, P. Allan; Mercier, David; Myatra, Sheila N.; O’Sullivan, Ellen P.; Rosenblatt, William H.; Sorbello, Massimiliano; Tung, Avery (2021-11-11). "2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway". Anesthesiology. 136 (1): 31–81. doi:10.1097/aln.0000000000004002. ISSN 0003-3022. PMID 34762729.
- ^ Patil, Susheel P.; Ayappa, Indu A.; Caples, Sean M.; Kimoff, R. John; Patel, Sanjay R.; Harrod, Christopher G. (2019-02-15). "Treatment of Adult Obstructive Sleep Apnea With Positive Airway Pressure: An American Academy of Sleep Medicine Systematic Review, Meta-Analysis, and GRADE Assessment". Journal of Clinical Sleep Medicine. 15 (2): 301–334. doi:10.5664/jcsm.7638. ISSN 1550-9389. PMC 6374080. PMID 30736888.
- ^ a b Gropper, Michael A., ed. (2020). Miller's anesthesia (Ninth ed.). Philadelphia, PA: Elsevier. ISBN 978-0-323-59604-6.
- ^ a b c d Goldman, Lee; Schafer, Andrew (2022). Goldman-Cecil Medicine (26th ed.). Elsevier. ISBN 9789752779259.
- ^ "Airway Obstruction". The Lecturio Medical Concept Library. Archived from the original on 2021-06-25. Retrieved 2021-06-25.
- ^ a b c d e "2024 GOLD Report". Global Initiative for Chronic Obstructive Lung Disease - GOLD. Retrieved 2024-11-08.
- ^ Balata, Haval; Harvey, Jonathan; Barber, Phil V; Colligan, Denis; Duerden, Rebecca; Elton, Peter; Evison, Matthew; Greaves, Melanie; Howells, John; Irion, Klaus; Karunaratne, Devinda (15 Jul 2020). "Spirometry performed as part of the Manchester community-based lung cancer screening programme detects a high prevalence of airflow obstruction in individuals without a prior diagnosis of COPD". Thorax. 75 (8): 655–660. doi:10.1136/thoraxjnl-2019-213584. ISSN 0040-6376. PMID 32444437. S2CID 218855570.
